Abstract
Introduction:
Intravascular Diffuse Large B-Cell Lymphoma (IV DLBCL) is a rare entity, with a generally aggressive course that may vary based on geographic presentation, and may be improving with modern diagnostic or therapeutic options. While a United States (US) registry study showed relatively good outcomes with IV DLBCL, clinicopathologic and treatment data were unavailable. We performed a detailed retrospective review of cases identified at 8 US medical centers, to improve understanding of IV DLBCL and inform management.
Methods:
We compiled data retrieved via IRB-approved review of IV DLBCL cases identified from 1999-2015 at eight academic institutions across the US. We characterized the cohort's clinical status at time of diagnosis, presenting diagnostic and clinical features of the disease, treatment modalities used, and overall prognostic data.
Results:
Fifty-three patients were identified, including thirty women and twenty-three. Median age was 63 years and with a median performance status (PS) at presentation of 2. The most common sites of diagnosis were brain (13), skin (11), and bone marrow (10). Presenting symptoms were variable but frequently included altered cognitive function with or without neurological deficits (12), rash (9), and dyspnea (8). At the time of diagnosis, 66% (29/44) of patients had accompanying B-symptoms.
The vast majority of patients presented with an elevated LDH (median 576 IQR 338-1459.8). The median International Prognostic Index (IPI) score at time of diagnosis was 4 (63% of patients presented with high risk disease). Fifty-Eight percent (25/43) of patients had bone marrow involvement, and 12% showed evidence of hemophagocytosis (5/41). Anemia (69%; 29/42) and thrombocytopenia (47%; 20/42) were the most common hematological abnormalities noted at time of presentation.
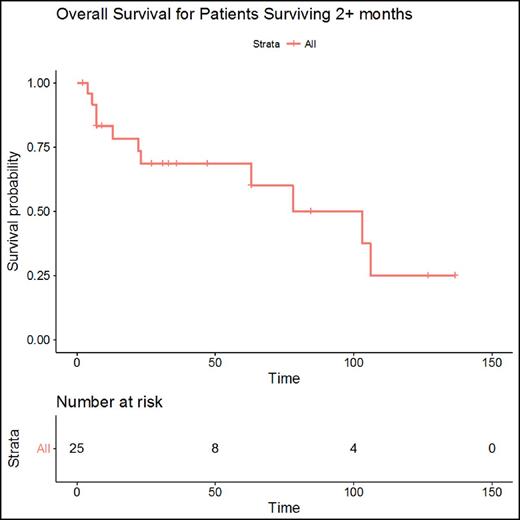
Initial treatment was known for 68% (36) pts. R-CHOP (20) was the most frequently given initial regimen from which 13 pts obtained CR with 5 undergoing consolidation with stem cell transplantation (ASCT). Other common initial regimens were CHOP (4) and R-CODOX (4) with CR obtained in 5 pts. Two patients received R-EPOCH (1) and R-hyperCVAD (1), both with CR followed by autologous SCT. The remaining regimens used were: R-DeAngelis (n=1 with PD), R-prednisone (n=1 with unknown response), R-dexamethasone (n=2 with PD), and high-dose steroids (n=1 with PD). Of these, 22 (61%) obtained complete response (CR), 7 (20%) had progressive disease (PD) and 4 (16%) had unknown response. Seven patients did not receive initial treatment and 10 patients had insufficient data. A single patient was diagnosed following organ removal and was treated with surgical excision alone with CR. For the 40 patients with information regarding survival time, 6 (15%) were diagnosed post-mortem, 9 (22.6%) survived 0-2 months and 25 (62.5%) had a survival of 2+ months. Eleven pts received a second line of therapy consisting of R-MVP, R-ESHAP, ICE, R-ICE and R-EPOCH, with 4 pts obtaining CR. 9 pts in the cohort went on to receive an ASCT; only two after 2nd line therapy. Of the 25 pts that achieved an overall survival of greater than 2 months, the median survival was 103 months (95% CI 63-NA).
Lower LDH and better (PS) at presentation was associated with improved survival but this is expected given that these are both factors within the IPI score, which was lower in the patients with survival greater than 2 months. While available data was limited there were no clear associations between survival and the cell of origin (Hans algorithm, n = 21) or expression of high risk markers, including CD5 (n=28), c-MYC (n=8), and BCL2 (n=15).
Conclusion: This represents the largest retrospective case series of IV DLBCL conducted at academic institutions in the US to date. In this 53 patient cohort, the most common presenting sites of IV DLBCL were brain, skin, and bone marrow. Overall survival was favorable in treated pts who survived longer than two months from diagnosis, suggesting that poor outcome in this disease may partly be attributable to difficulty diagnosing IV DLBCL early enough to administer therapy. Lower IPI score, in particular lower ECOG PS and LDH were associated with improved survival. While CR was achieved in the majority of treated patients, more data is needed to determine whether durability of responses and OS are more attributable to time to diagnosis, specific treatment regimens, or as yet unknown difference in disease biology.
Smith:Sharp: Research Funding; Merck: Research Funding; Seattle Genetics: Research Funding; Dohme Corp: Research Funding; Janssen: Research Funding; Acerta: Research Funding; Pharmacyclics LLC, an AbbVie Company: Research Funding; Genentech: Research Funding; Portola Pharmaceuticals: Research Funding. Kaplan:Janssen, Seattle Genetics, Millennium Pharmaceuticals, Inc., a wholly owned subsidiary of Takeda Pharmaceutical Company Limited: Research Funding. Barr:Seattle Genetics: Consultancy; Gilead: Consultancy; Infinity: Consultancy; Novartis: Consultancy; Celgene: Consultancy; AbbVie: Consultancy, Research Funding; Pharmacyclics LLC, an AbbVie Company: Consultancy, Research Funding. Caimi:Abbvie: Equity Ownership; Incyte: Equity Ownership; Celgene: Speakers Bureau; Seattle Genetics: Equity Ownership. Herrera:Pharmacyclics: Consultancy, Research Funding; Seattle Genetics: Research Funding; Merck: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Genentech: Consultancy, Research Funding; Immune Design: Research Funding. Phillips:Incyte: Other: Travel/Expenses; Seattle Genetics: Consultancy; KITE: Consultancy; Pharmacyclics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal